NIH-backed startup Amissa launches AI infrastructure for menopause care, tackling a $24.8bn data blindspot
Designed as clinical intelligence and documentation support.
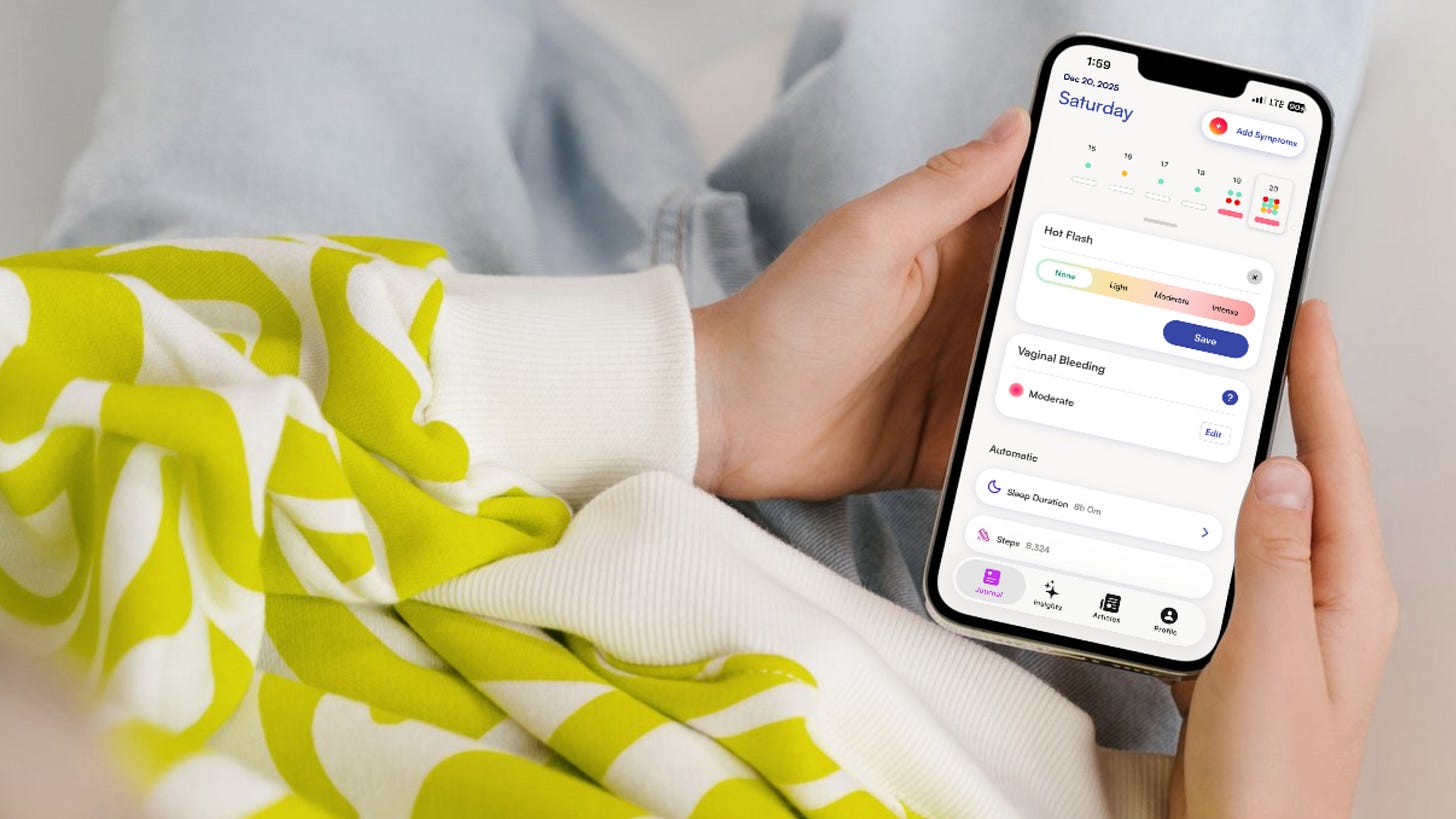
As perimenopause and menopause awareness has grown in recent years, the importance of symptom tracking has grown with it. Women have been encouraged to keep records of what they are experiencing to help with advocating for themselves during appointments, spotting their own patterns and supporting diagnosis.
Yet this symptom tracking can still be inconsistent - hot flushes here, sleep problems there - the reporting can often still rely on memory rather than data, and what is recorded will usually sit with the patient on their phone or notepad rather than with the clincian. That means care ends up being episodic, documentation inconsistent and the condition rarely treated as the long-term health transition it is.
A new NIH-backed startup, Amissa, wants to change that.
Launched this week, Amissa describes itself as the first clinical intelligence platform built specifically for menopause. Previously the recipient of an NIH grant, it is now already live in 10 early adopter practices across the U.S., and aims to give clinicians something they have never really had before: a clear, longitudinal picture of what a patient is experiencing over time.
Instead of relying on what a patient can recall in a ten-minute appointment, clinicians using Amissa include a standardised menopause assessment as part of intake or pre-visit workflows. Patients record symptoms and severity in the app and, if they use a wearable such as an Apple Watch, Oura, Garmin or Whoop, that data can be pulled in too. Wearables are optional – the core of the system is structured symptom tracking.
All of that information is then pulled together into a concise, “visit-ready” summary for the clinician.
“Amissa is the only platform built with clinicians, for clinicians, to make menopause symptom data actionable,” said Samantha Smith, Co-Founder and CEO of Amissa.
“We connect providers directly to objective patient data and turn it into insight they can actually use in care.”
Unmanaged symptoms
Menopause and perimenopause affect more than 75 million women in the US and are linked to almost $25bn in excess healthcare spending each year. Much of that cost stems from symptoms that go unrecognised, unrecorded or unmanaged. The result is repeated appointments, misdirected referrals and years of frustration for patients.
“Menopause symptoms don’t move in a straight line,” said Dr Ariel Haddad, an OB-GYN and founder of Helia Health, one of the early adopters.
“When I can see what’s improving, what’s worsening and what’s staying the same between visits, I can adjust care with confidence and show patients that their experience is being taken seriously.”
Until now, much of menopause innovation has sat outside the healthcare system, in consumer apps and employer programmes. Amissa is explicitly trying to build infrastructure inside clinical care.
“Menopause isn’t a moment – it’s a decade-long health transition,” Smith said. “The companies that win this market will be the ones that own the underlying data infrastructure. That’s what we’re building.”
Structured intelligence that surfaces patterns
At the heart of the platform is an AI layer that organises and structures the data. It does not diagnose, make decisions or recommend treatment. Instead, it highlights patterns, changes over time and clinically relevant signals, and turns messy, free-text symptom reports into standardised outputs that fit real clinical workflows.
And while wearable integrations are already available, this is not a blocker for those who don’t have one.
“Amissa is built to be accessible to all women – not just the data-obsessed,” Smith told FutureFemHealth.
“Clinicians include our standardised assessment as part of intake, calculating symptom severity and introducing our tracking tools through the app. If a patient uses a wearable, we incorporate that too. Everything comes together in a short summary that helps clinicians quickly understand what’s changing and what matters most for the visit.”
Looking ahead
The AI behind Amissa’s platform will evolve over time - the team has been working inside live practices since last summer, using real clinical settings to refine how information is summarised and presented. Over time, it plans to extend those capabilities to patient-facing insights, but Smith says clinical validation and guardrails remain central.
With NIH backing and early uptake across 10 practices, Amissa is betting that the future of menopause care lies not in another wellness product, but in making an invisible life stage measurable, trackable and legible to medicine itself.