The role of digital therapeutics for hormonal health conditions
How do digital therapeutics deliver care through technology?
A guest post from Victoria Schoeffel, co-founder of Belle Health, a digital app that combines cycle tracking, symptom management, and CBT tools to help individuals better manage premenstrual disorders.
With growing demand for more personalized and accessible care, digital health solutions are increasingly transforming the way we manage, treat, and understand chronic conditions.
At the forefront of this shift is the rise of Digital Therapeutics (DTx)—evidence-based, software-driven medical interventions. Unlike traditional approaches, DTx delivers care through technology, empowering individuals while addressing gaps in healthcare delivery.
This transformation is particularly promising for hormonal health, a historically under-researched and underserved area affecting millions of women and individuals assigned female at birth (AFAB) worldwide. By blending science, technology, and innovation, DTx is unlocking new possibilities for managing hormonal health conditions.
In this article, we’ll explore how digital therapeutics work and how they differ from wellness apps, why digital therapeutics can support hormonal health and how Belle Health is developing a research-backed internet-based cognitive-behavioral therapy (iCBT) program specifically tailored to PMDD.
What are digital therapeutics (DTx)?
Digital therapeutics (DTx) are a category of software-based healthcare solutions designed to deliver evidence-based medical interventions. These tools aim to prevent, manage, or treat specific diseases and conditions by leveraging the power of technology.
Unlike general health apps, which primarily focus on fitness or wellness, DTx products are clinically validated and often regulated as medical devices, ensuring they meet stringent standards for safety, efficacy, and reliability.
Digital therapeutics therefore stand at the intersection of medicine and technology, combining advanced software capabilities with scientific rigor. They often integrate seamlessly with traditional healthcare pathways and are designed to work independently or as adjuncts to conventional treatments such as medications or in-person therapies. Their goal is to provide personalized, scalable, and effective care, improving patient outcomes and reducing the burden on healthcare systems.
Core features of digital therapeutics
1. Clinical validation and evidence-based design
Digital therapeutics undergo rigorous clinical testing, including randomized controlled trials, to validate their safety and efficacy. This ensures that their interventions are supported by scientific evidence, aligning with the same standards used for pharmaceutical drugs and medical devices.
2. Regulatory oversight
Many DTx solutions are regulated by health authorities like the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), or similar bodies worldwide. This regulation ensures that these products meet stringent medical device standards for effectiveness, data security, and patient safety.
3. Personalization and adaptive interventions
DTx utilizes advanced algorithms, artificial intelligence, and real-time data to deliver interventions tailored to an individual’s unique medical history, behavior patterns, and health needs. This level of personalization enhances the effectiveness of treatment and user engagement.
4. Integrated and measurable care
Unlike wellness apps, which offer generic advice, DTx solutions provide structured, measurable outcomes. They are often integrated with healthcare systems, allowing for seamless data sharing with healthcare providers, enabling better monitoring and decision-making.
5. Data-Driven Insights
DTx harness data from multiple sources, including wearables, mobile devices, and user inputs, to deliver actionable insights. For instance, they can track physiological metrics like heart rate, glucose levels, or sleep patterns to inform and adjust therapeutic interventions dynamically.
6. Behavioral Change Support
Many DTx platforms incorporate behavioral science principles, including cognitive-behavioral therapy (CBT), gamification, and habit formation strategies. These features empower users to make lasting lifestyle changes that improve their health outcomes.
7. Accessibility and Scalability
Digital therapeutics can be delivered via smartphones, tablets, or web platforms, making them accessible to a wide range of users. Their scalability allows for cost-effective deployment, especially in underserved or remote areas where access to healthcare may be limited.
How do digital therapeutics differ from wellness apps
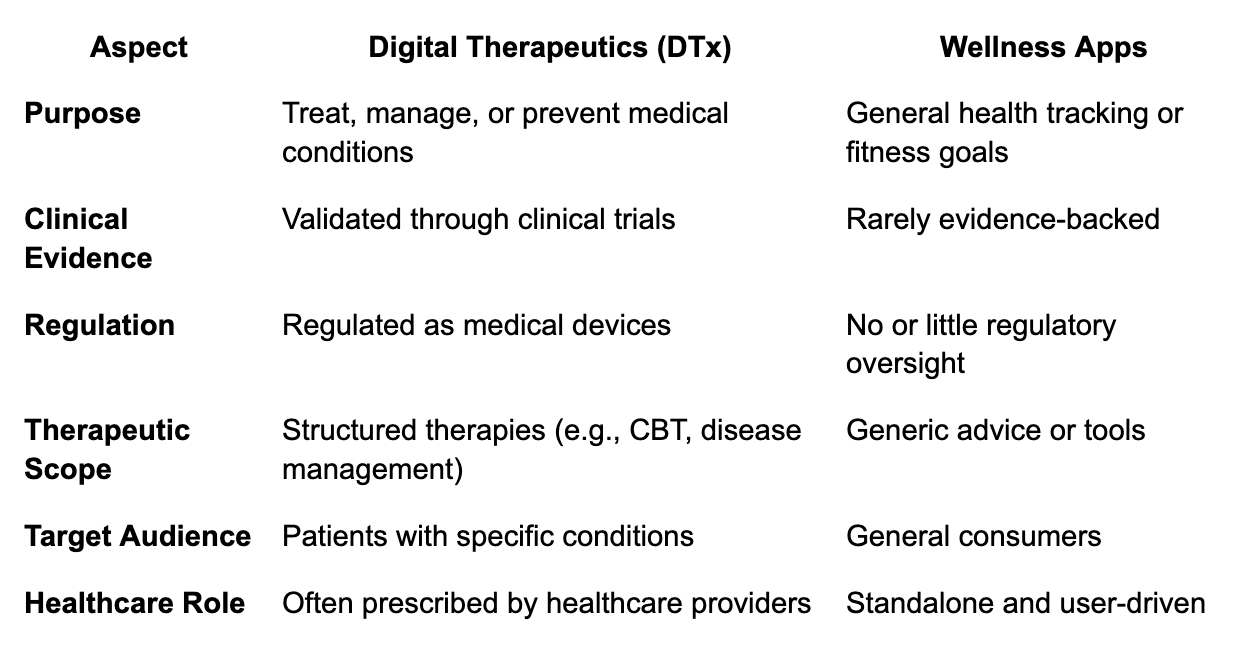
Digital therapeutics are fundamentally distinct from standard wellness apps in their design, purpose, and impact. While wellness apps focus on general health and fitness, DTx targets specific medical conditions with clinical-grade interventions. The table below highlights the key differences:
This combination of scientific validation, regulatory approval, and targeted therapeutic interventions positions digital therapeutics as a transformative tool in modern medicine, bridging gaps in traditional healthcare delivery and enhancing outcomes for patients worldwide.
Digital therapeutics have transformed disease management through evidence-based digital interventions. These solutions excel in chronic disease management by monitoring real-time data, providing personalized recommendations, and supporting behavioral changes. In diabetes care, DTx tracks glucose levels and offers dietary guidance, while in mental health, it delivers cognitive-behavioral therapy for conditions like anxiety and depression. Applications extend to chronic pain, cardiovascular health, and sleep disorders, with FDA-approved platforms demonstrating how digital therapeutics make precision care accessible, scalable, and personalized.
Why digital therapeutics make sense for hormonal health conditions
Hormonal health conditions such as PMDD, PCOS, and menopause-related symptoms represent a critical area where digital therapeutics (DTx) can make a transformative impact. That’s because these conditions often involve a significant psychological component—manifesting as mood swings, anxiety, depression, or sleep disturbances—that traditional healthcare approaches struggle to address adequately.
These conditions are also severely undertreated due to systemic gaps in care, including a lack of access to specialists, fragmented treatment approaches, and limited awareness. Digital therapeutics are uniquely positioned to address these challenges by providing targeted, evidence-based interventions that leverage therapies proven effective for these conditions without traditional barriers to access.
DTx platforms draw upon therapies like cognitive-behavioral therapy (CBT), psychoeducation, and mindfulness, which have shown measurable success in managing the psychological and emotional symptoms of hormonal health conditions. Unlike traditional care models, which may rely on sporadic clinic visits or medication alone, digital therapeutics integrate these therapies seamlessly into daily life, offering structured, interactive support directly through devices. For hormonal health, this integration makes DTx not just a complementary tool but the next logical wave of innovation, filling the gaps left by the current healthcare system in a scalable and patient-centric manner.
Why hormonal health is the next wave for digital therapeutics
Digital therapeutics are particularly well-suited for hormonal health because they focus on therapies that address the root causes of distress, such as the interplay between hormonal fluctuations and mental health. For example, individuals with PMDD benefit from DTx platforms that provide CBT exercises designed to reframe negative thought patterns, symptom tracking to predict mood swings, and actionable recommendations for self-care. Similarly, for menopause-related symptoms, platforms can deliver personalized interventions targeting sleep disturbances, memory fog, and mood instability, improving overall well-being without the need for invasive treatments.
What makes DTx revolutionary in this space is their ability to overcome barriers that often prevent individuals from accessing care. They require no physical infrastructure, making them accessible in underserved areas, and they provide on-demand, consistent support tailored to the user’s specific needs. For hormonal health, this is especially crucial as these conditions affect millions globally, yet often go untreated due to stigma or systemic gaps in care.
By focusing on therapies that have already proven effective and scaling them through digital platforms, DTx are not just an innovative solution—they are a necessity. As hormonal health continues to gain recognition as a critical area of care, digital therapeutics stand ready to lead the charge, providing the accessibility, personalization, and holistic support that traditional systems have yet to achieve.
Case study: A digital therapeutics for PMDD
Premenstrual Dysphoric Disorder (PMDD) is a severe condition affecting around 5% of women and AFAB individuals of reproductive age, leading to debilitating physical and emotional symptoms that can significantly disrupt daily life.
Despite its prevalence, PMDD is underdiagnosed and undertreated due to a lack of awareness and limited access to specialized care. Recognizing these challenges, Professor Cornelia Weise and Professor Maria Kleinstäuber developed an internet-based cognitive-behavioral therapy (iCBT) program specifically tailored to PMDD. Their clinical trial, involving 174 participants, demonstrated that the iCBT intervention significantly reduced symptom intensity, functional impairment, and psychological distress compared to a control group, with lasting benefits observed at a six-month follow-up.
Building on this research, Belle Health collaborated with Professors Weise and Kleinstäuber to translate their validated iCBT program into a digital therapeutic platform. This app integrates the structured iCBT framework with hormonal tracking technology, allowing users to monitor their cycles, receive personalized interventions, and manage their symptoms proactively. Belle Health is now validating these results through additional clinical trials, conducted in collaboration with the original research team, to ensure the platform’s efficacy and scalability.
The digital therapeutic approach is particularly well-suited for PMDD because it addresses critical gaps in care. Access to PMDD specialists is scarce, leaving many individuals without adequate treatment. A digital platform eliminates these barriers by delivering evidence-based care directly to users, making it accessible to those in underserved or remote areas. Moreover, the integration of psychological therapies like iCBT, which are proven effective for PMDD, into a scalable digital tool ensures consistent, user-centered support. This combination of accessibility, personalization, and clinical validation positions digital therapeutics as an essential solution for managing PMDD and improving the lives of those affected.
Conclusion: The future of hormonal health with digital therapeutics
Digital therapeutics are redefining how we understand and manage hormonal health, providing scalable, evidence-based solutions for conditions like PMDD, PCOS, and menopause-related symptoms. By addressing critical gaps in care, these tools empower individuals to take control of their health while making expert care accessible to underserved populations.
For conditions with strong psychological and cyclical components, like PMDD, digital therapeutics offer a tailored approach that combines symptom tracking, cognitive-behavioral therapy, and real-time interventions. These solutions not only enhance individual outcomes but also reduce the systemic burden on healthcare systems by offering efficient, scalable alternatives to traditional care.